For Healthcare Providers

With over 26 years of established clinical success, low-intensity pulsed ultrasound (LIPUS) devices have been shown to accelerate fracture repair and enhance non-union healing.4-7
How does LIPUS work?
Low-intensity pulsed ultrasound (LIPUS) medical devices use ultrasound waves to create nano-motion at the fracture site that stimulates a biochemical response through integrin mechano-receptors by enhancing the production of cyclo-oxygenase 2 (COX-2) that triggers molecules to enhance fracture repair.2
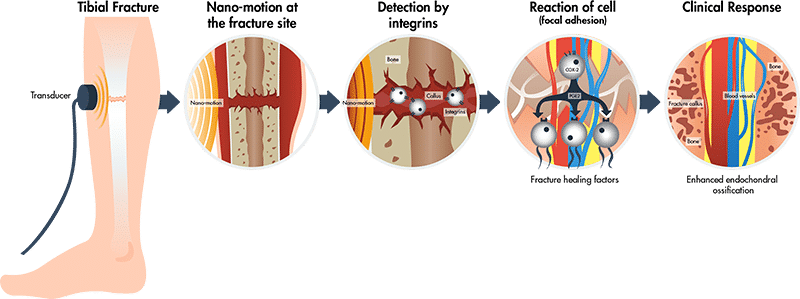
Adapted from Harrison A, Lin S, Pounder N, Mikuni-Takagaki Y. Ultrasonics. 2016;70:45-52.
COX-2=cyclo-oxygenase 2; PGE2=prostaglandin E2
Key clinical trials supporting LIPUS device treatment
(Double-blind RCT)
(Double-blind RCT)
(Self-pairing)
(Registry)
(Double-blind RCT)
Treatment
LIPUS device for 20 mins per day (n=33) vs. Placebo (n=34)
Lipus Device Studied
Ie: 30 mW/cm2
faw: 1.5 MHz
PRF: 1 kHz
PW: 200 μs
Type and Location of Fracture
Fresh fractcure (<7 days)
Tibia
Demographics
- Skeletally mature men and non-pregnant women
- <76 years old
Key Results
Decrease in time to overall healing: 96 ± 4.9 days vs. 154 ± 13.7 days, p=0.0001
~38% faster healing with LIPUS device vs. placebo
Reference
Heckman JD, Ryaby JP, McCabe J, et al. J Bone Joint Surg Am. 1994;76(1):26-34.
Aer=effective radiating area; DF=duty cycle (duty factor); faw= ultrasound frequency or frequency Sine waves; Ie=effective intensity (spatial average temporal average); P=temporal average power; PRF=pulse repetition frequency (repetition rate/modulation frequency); PW=pulse duration (signal burst or signal burst width, pulse burst width, modulating signal burst width); Q=beam type; Rbn=beam non-uniformity ratio
(Double-blind RCT)
Treatment
LIPUS device for 20 mins per day (n=30) vs. Placebo (n=31)
Lipus Device Studied
Ie: 30 mW/cm2
faw: 1.5 MHz
PRF: 1 kHz
PW: 200 μs
DF: 20%
Type and Location of Fracture
Fresh fracture (<7 days)
Radius
Demographics
- Men and non-pregnant women
- >21 years old
- Included smokers
Key Results
Time to union: 61 ± 3 days vs. 98 ± 5 days, p<0.0001
~38% faster time to union with LIPUS device vs. placebo
Reference
Kristiansen TK, Ryaby JP, McCabe J, et al. J Bone Joint Surg Am. 1997;79(7):961-973.
Aer=effective radiating area; DF=duty cycle (duty factor); faw= ultrasound frequency or frequency Sine waves; Ie=effective intensity (spatial average temporal average); P=temporal average power; PRF=pulse repetition frequency (repetition rate/modulation frequency); PW=pulse duration (signal burst or signal burst width, pulse burst width, modulating signal burst width); Q=beam type; Rbn=beam non-uniformity ratio
(Self-pairing)
Treatment
LIPUS device for 20 mins per day (n=29)
Lipus Device Studied
Ie: 30 mW/cm2
faw: 1.5 MHz
PRF: 1 kHz
PW: 200 μs
DF: 20%
Type and Location of Fracture
Non-unions (failure to unite >6 months from fracture) on:
- Tibia
- Femur
- Radius/ulna
- Scaphoid
- Humerus
- Metatarsal
- Clavicle
Average non-union fracture age is 61 weeks.
Demographics
- Men and non-pregnant women
- 18-90 years old
- Included smokers
Key Results
25 of 29 non-union cases healed in an average time of 22 weeks.
~86% healed
Reference
Nolte PA, van der Krans A, Patka P, et al. J Trauma. 2001;51(4):693-703.
Aer=effective radiating area; DF=duty cycle (duty factor); faw= ultrasound frequency or frequency Sine waves; Ie=effective intensity (spatial average temporal average); P=temporal average power; PRF=pulse repetition frequency (repetition rate/modulation frequency); PW=pulse duration (signal burst or signal burst width, pulse burst width, modulating signal burst width); Q=beam type; Rbn=beam non-uniformity ratio
(Registry)
Treatment
LIPUS device (n=4,190)
Lipus Device Studied
Ie: 30 ± 30% mW/cm2
faw: 1.5 ± 5% MHz
PRF: 1.0 ± 10% kHz
PW: 200 ± 10% µs
DF: 20%
Aer: 3.88 ± 1% cm2
P: 117 mW (±30%)
RBN: 4.0 maximum
Q: Collimated
Type and Location of Fracture
Fresh fracture (≤90 days old)
- Tibia
- Fibula
- Femur
- Metatarsal
- Radius
- Humerus
- Scaphoid
- Clavicle
- Ankle
- Ulna
- Metacarpal
Closed fractures (n=3,212)
Open fractures (n=147)
Demographics
- Men and women
Included comorbidities:
- Smoking
- Diabetes
- Hypertension
- Vascular insufficiency
- Osteoporosis
- Cancer
- Cardiovascular disease
- Alcoholism
- Renal disease
- Rheumatoid arthritis
Key Results
Heal rate:
>94% healed
Elderly (≥60 years old) had similar heal rate to the population as a whole.
Days to treatment was significantly shorter for patients who healed (38.3 [±24.3] mean days) vs. those who failed (47.1 [±27.3] mean days), p=0.0001; (earlier treatment provides better outcomes).
Reference
Zura R, Mehta S, Della Rocca GJ, et al. BMC Musculoskelet Disord. 2015;16:45-55.
Aer=effective radiating area; DF=duty cycle (duty factor); faw= ultrasound frequency or frequency Sine waves; Ie=effective intensity (spatial average temporal average); P=temporal average power; PRF=pulse repetition frequency (repetition rate/modulation frequency); PW=pulse duration (signal burst or signal burst width, pulse burst width, modulating signal burst width); Q=beam type; Rbn=beam non-uniformity ratio
UNIO Technical Specifications
Ie: 30 ± 30% mW/cm2
P: 117 ± 20% mW
RBN: 4.0 Max
Aer: 3.88 ± 5% cm2
ƒawf: 1.5 ± 5% MHz
Waveform: Pulsed
PW: 200 ± 5% μs
PRF: 1.0 ± 5% kHz
DF: 20%
Q: Collimated
Why UNIO for your patients?

HEALTH CANADA APPROVED
UNIO is a Health Canada approved Class II medical device (Licence No. 109919) indicated for the treatment of fresh bone fractures and established non-unions excluding treatment of the skull and vertebral column.
EASY-TO-USE AT HOME

ACCELERATES HEALING
What type of patients can use UNIO?
UNIO is indicated for treatment of fresh bone fractures and established non-unions excluding treatment of the skull and vertebral column. The location and type of fracture will influence results.1
The UNIO device can be used in the presence of metal screws and plates.1
The UNIO device is intended for non-invasive use only, and must only be used as prescribed by a physician or other Medical Professional for its intended use, in accordance with the UNIO User Guide.1
People with cardiac pacemakers should get clearance from their physician prior to use.1
Evidence of safety and efficacy has not been established in certain populations. Refer to the UNIO User Guide for more information.
Email UNIO to receive a EN/FR copy of the user guide at [email protected]
How do I get my patients started with UNIO?
UNIO must be prescribed by a Physician or Medical Professional. Please contact us for more information on how to prescribe for your patients.